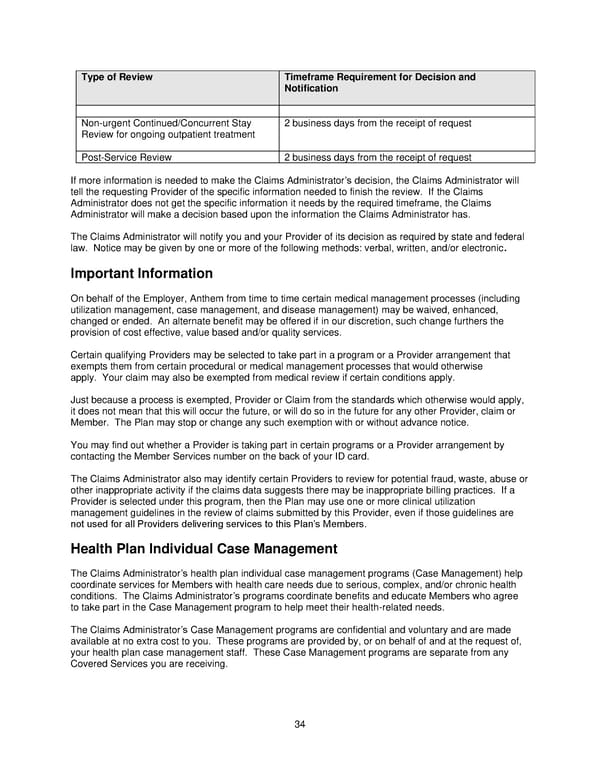
34 Type of Review Timeframe Requirement for Decision and Notification Non-urgent Continued/Concurrent Stay Review for ongoing outpatient treatment 2 business days from the receipt of request Post-Service Review 2 business days from the receipt of request If more information is needed to make the Claims Administrator’s decision, the Claims Administrator will tell the requesting Provider of the specific information needed to finish the review. If the Claims Administrator does not get the specific information it needs by the required timeframe, the Claims Administrator will make a decision based upon the information the Claims Administrator has. The Claims Administrator will notify you and your Provider of its decision as required by state and federal law. Notice may be given by one or more of the following methods: verbal, written, and/or electronic. Important Information On behalf of the Employer, Anthem from time to time certain medical management processes (including utilization management, case management, and disease management) may be waived, enhanced, changed or ended. An alternate benefit may be offered if in our discretion, such change furthers the provision of cost effective, value based and/or quality services. Certain qualifying Providers may be selected to take part in a program or a Provider arrangement that exempts them from certain procedural or medical management processes that would otherwise apply. Your claim may also be exempted from medical review if certain conditions apply. Just because a process is exempted, Provider or Claim from the standards which otherwise would apply, it does not mean that this will occur the future, or will do so in the future for any other Provider, claim or Member. The Plan may stop or change any such exemption with or without advance notice. You may find out whether a Provider is taking part in certain programs or a Provider arrangement by contacting the Member Services number on the back of your ID card. The Claims Administrator also may identify certain Providers to review for potential fraud, waste, abuse or other inappropriate activity if the claims data suggests there may be inappropriate billing practices. If a Provider is selected under this program, then the Plan may use one or more clinical utilization management guidelines in the review of claims submitted by this Provider, even if those guidelines are not used for all Providers delivering services to this Plan’s Members. Health Plan Individual Case Management The Claims Administrator’s health plan individual case management programs (Case Management) help coordinate services for Members with health care needs due to serious, complex, and/or chronic health conditions. The Claims Administrator’s programs coordinate benefits and educate Members who agree to take part in the Case Management program to help meet their health-related needs. The Claims Administrator’s Case Management programs are confidential and voluntary and are made available at no extra cost to you. These programs are provided by, or on behalf of and at the request of, your health plan case management staff. These Case Management programs are separate from any Covered Services you are receiving.
 2025 Retiree Indemnity Plan Booklet Page 34 Page 36
2025 Retiree Indemnity Plan Booklet Page 34 Page 36