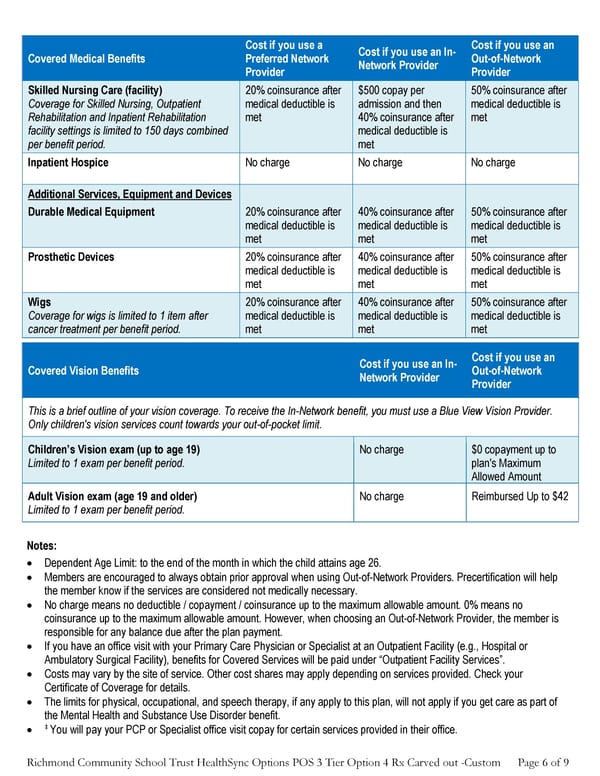
Richmond Community School Trust HealthSync Options POS 3 Tier Option 4 Rx Carved out -Custom Page 6 of 9 Covered Medical Benefits Cost if you use a Preferred Network Provider Cost if you use an In- Network Provider Cost if you use an Out-of-Network Provider Skilled Nursing Care (facility) Coverage for Skilled Nursing, Outpatient Rehabilitation and Inpatient Rehabilitation facility settings is limited to 150 days combined per benefit period. 20% coinsurance after medical deductible is met $500 copay per admission and then 40% coinsurance after medical deductible is met 50% coinsurance after medical deductible is met Inpatient Hospice No charge No charge No charge Additional Services, Equipment and Devices Durable Medical Equipment 20% coinsurance after medical deductible is met 40% coinsurance after medical deductible is met 50% coinsurance after medical deductible is met Prosthetic Devices 20% coinsurance after medical deductible is met 40% coinsurance after medical deductible is met 50% coinsurance after medical deductible is met Wigs Coverage for wigs is limited to 1 item after cancer treatment per benefit period. 20% coinsurance after medical deductible is met 40% coinsurance after medical deductible is met 50% coinsurance after medical deductible is met Covered Vision Benefits Cost if you use an In- Network Provider Cost if you use an Out-of-Network Provider This is a brief outline of your vision coverage. To receive the In-Network benefit, you must use a Blue View Vision Provider. Only children's vision services count towards your out-of-pocket limit. Children’s Vision exam (up to age 19) Limited to 1 exam per benefit period. No charge $0 copayment up to plan's Maximum Allowed Amount Adult Vision exam (age 19 and older) Limited to 1 exam per benefit period. No charge Reimbursed Up to $42 Notes: • Dependent Age Limit: to the end of the month in which the child attains age 26. • Members are encouraged to always obtain prior approval when using Out-of-Network Providers. Precertification will help the member know if the services are considered not medically necessary. • No charge means no deductible / copayment / coinsurance up to the maximum allowable amount. 0% means no coinsurance up to the maximum allowable amount. However, when choosing an Out-of-Network Provider, the member is responsible for any balance due after the plan payment. • If you have an office visit with your Primary Care Physician or Specialist at an Outpatient Facility (e.g., Hospital or Ambulatory Surgical Facility), benefits for Covered Services will be paid under “Outpatient Facility Services”. • Costs may vary by the site of service. Other cost shares may apply depending on services provided. Check your Certificate of Coverage for details. • The limits for physical, occupational, and speech therapy, if any apply to this plan, will not apply if you get care as part of the Mental Health and Substance Use Disorder benefit. • ‡ You will pay your PCP or Specialist office visit copay for certain services provided in their office.
 Anthem Summary of Benefits PPO Plan Page 5 Page 7
Anthem Summary of Benefits PPO Plan Page 5 Page 7