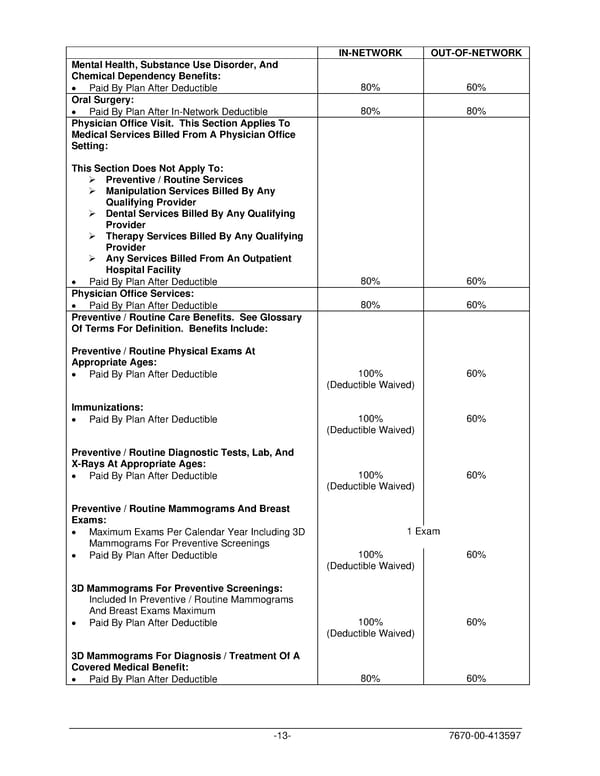
IN-NETWORK OUT-OF-NETWORK Mental Health, Substance Use Disorder, And Chemical Dependency Benefits: • Paid By Plan After Deductible 80% 60% Oral Surgery: • Paid By Plan After In-Network Deductible 80% 80% Physician Office Visit. This Section Applies To Medical Services Billed From A Physician Office Setting: This Section Does Not Apply To: ➢ Preventive / Routine Services ➢ Manipulation Services Billed By Any Qualifying Provider ➢ Dental Services Billed By Any Qualifying Provider ➢ Therapy Services Billed By Any Qualifying Provider ➢ Any Services Billed From An Outpatient Hospital Facility • Paid By Plan After Deductible 80% 60% Physician Office Services: • Paid By Plan After Deductible 80% 60% Preventive / Routine Care Benefits. See Glossary Of Terms For Definition. Benefits Include: Preventive / Routine Physical Exams At Appropriate Ages: • Paid By Plan After Deductible 100% 60% (Deductible Waived) Immunizations: • Paid By Plan After Deductible 100% 60% (Deductible Waived) Preventive / Routine Diagnostic Tests, Lab, And X-Rays At Appropriate Ages: • Paid By Plan After Deductible 100% 60% (Deductible Waived) Preventive / Routine Mammograms And Breast Exams: • Maximum Exams Per Calendar Year Including 3D 1 Exam Mammograms For Preventive Screenings • Paid By Plan After Deductible 100% 60% (Deductible Waived) 3D Mammograms For Preventive Screenings: Included In Preventive / Routine Mammograms And Breast Exams Maximum • Paid By Plan After Deductible 100% 60% (Deductible Waived) 3D Mammograms For Diagnosis / Treatment Of A Covered Medical Benefit: • Paid By Plan After Deductible 80% 60% -13- 7670-00-413597
 PLAN 01 01 2024 00 Page 15 Page 17
PLAN 01 01 2024 00 Page 15 Page 17