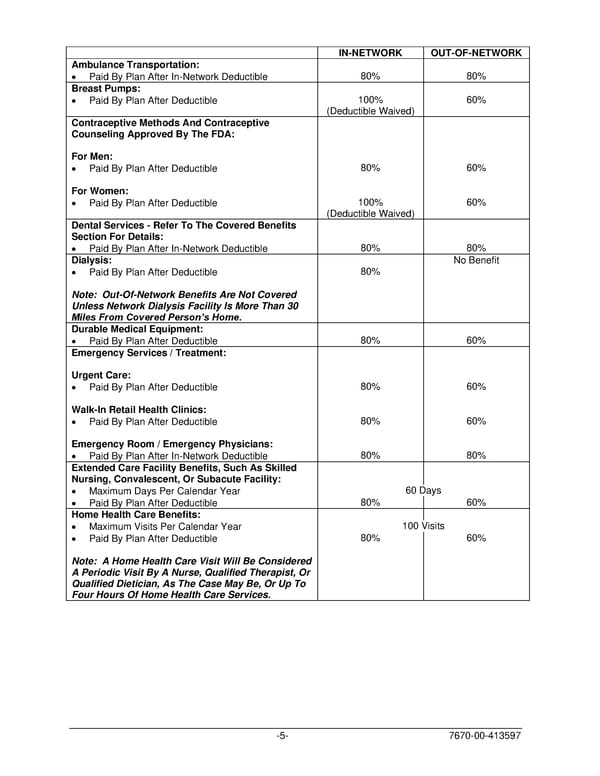
IN-NETWORK OUT-OF-NETWORK Ambulance Transportation: • Paid By Plan After In-Network Deductible 80% 80% Breast Pumps: • Paid By Plan After Deductible 100% 60% (Deductible Waived) Contraceptive Methods And Contraceptive Counseling Approved By The FDA: For Men: • Paid By Plan After Deductible 80% 60% For Women: • Paid By Plan After Deductible 100% 60% (Deductible Waived) Dental Services - Refer To The Covered Benefits Section For Details: • Paid By Plan After In-Network Deductible 80% 80% Dialysis: No Benefit • Paid By Plan After Deductible 80% Note: Out-Of-Network Benefits Are Not Covered Unless Network Dialysis Facility Is More Than 30 Miles From Covered Person’s Home. Durable Medical Equipment: • Paid By Plan After Deductible 80% 60% Emergency Services / Treatment: Urgent Care: • Paid By Plan After Deductible 80% 60% Walk-In Retail Health Clinics: • Paid By Plan After Deductible 80% 60% Emergency Room / Emergency Physicians: • Paid By Plan After In-Network Deductible 80% 80% Extended Care Facility Benefits, Such As Skilled Nursing, Convalescent, Or Subacute Facility: • Maximum Days Per Calendar Year 60 Days • Paid By Plan After Deductible 80% 60% Home Health Care Benefits: • Maximum Visits Per Calendar Year 100 Visits • Paid By Plan After Deductible 80% 60% Note: A Home Health Care Visit Will Be Considered A Periodic Visit By A Nurse, Qualified Therapist, Or Qualified Dietician, As The Case May Be, Or Up To Four Hours Of Home Health Care Services. -5- 7670-00-413597
 PLAN 01 01 2024 00 Page 7 Page 9
PLAN 01 01 2024 00 Page 7 Page 9